How you can proof that your digital health solution improves outcomes
The competition among digital health is rising. And it’s rising fast. One of the ways to stay ahead of the competition is to sign (big) contracts with (big) payors. But that's easier said than done. Signing contracts with one payor is difficult, but signing contracts with multiple payors is a completely different ballgame.
The most important thing you can do to get payor contracts is gathering evidence. Evidence that you reduce costs. Evidence that you improve outcomes. Evidence that they boost the patient experience.
Before approaching payors, ask yourself 3 questions:
Does my solution reduce costs?
Does my solution improve outcomes?
Does my solution boost patient experience?
A flowchart that guides you through these questions could look like this:
I have spoken with several people who have experience negotiating payors' contracts in the last few weeks. Each of them agreed: cost reduction is still the most critical factor when deciding whether they decide to sign a deal or not. So, If payors would prioritize these three things, it will probably look like this:
Reduce costs
Improve outcomes
Boost patient experience
Selling directly to businesses may change these priorities. The patient experience could be more important than a reduction in costs. But this depends from industry to industry. Is the patient experience more important to big tech companies than cost reduction? Probably. Is the patient experience more important to big manufacturers than cost reduction? I doubt it.
You’re probably thinking: yeah cool. But how can you prove that you have a positive impact on outcomes? What if I’m only in an MVP state or that I only have 100 MAUs? To solve this question, many digital health startups start as direct-to-consumer businesses. They start to gather evidence that they improve outcomes as a D2C company. Once they have this evidence, they eventually become B2C companies or B2B2C entities.
But how do you gather this evidence? I sat down with Tamra Lair, Chief Analytics Officer at Bind Benefits and a real thought leader when it comes to this, and she defined 3 crucial steps.
*The following sections are a combination of the conversation I had with Tamra, input from Chris Turtizin, Josh Heurung and my own experiences with collecting patient outcomes.*
Step 1: Develop an outcome framework
For the ease of this piece, I use ‘outcomes ‘ as a general term for health outcomes, costs and patient experience TL: “An outcome framework should clarify exactly what you want to prove over time. And it should be defined before you start collecting any data. In this framework, you will make a summary of all the data that you will capture to prove your product value. It must contain outcomes that matter to your patient population, and outcomes that matter to payors and employers.”
While defining this framework, It’s important that you focus on outcomes and not outputs:
Outputs are a quantitative summary of activities (e.g the number of patient consultations per year)
Outcomes focus on the value that occurs from delivering that activity (e.g improved patient satisfaction following their consultation)
Engagement with patients is crucial to identifying outcomes that matter to them. When it comes to finding out what outcomes matter to employers and payors, the same is true. Thus, you will have to speak to patients, employers, and payers. Find out what outcomes matter to them, what improvements they would like to see and what success would look like for them.
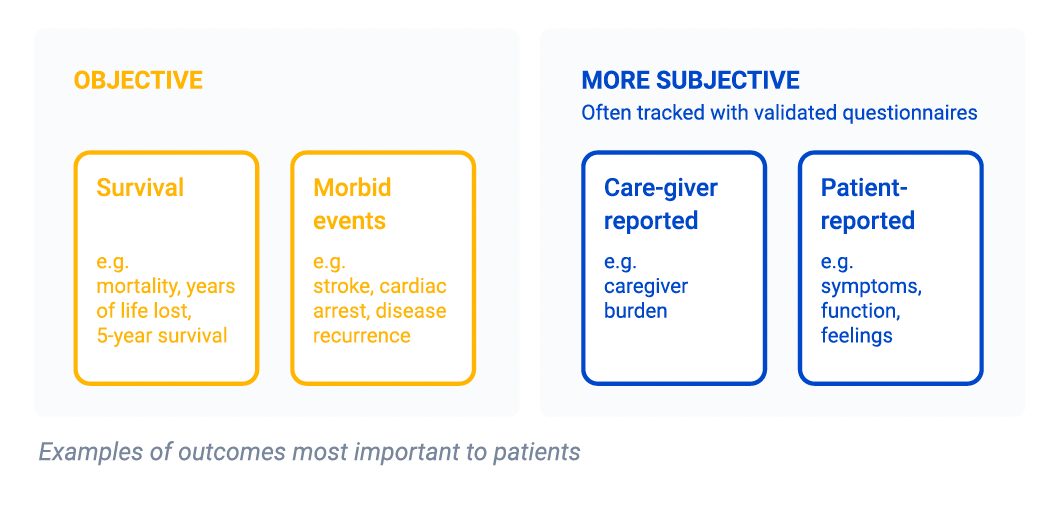
You have 2 types of outcomes:
Objective outcomes are observable, factual and can be assessed by everyone (e.g 5-year survival rates)
Subjective outcomes are those reported by patients and assessable by one but the patient, and they’re tracked most often using valid questionnaires (e.g patient feelings and symptoms)
To achieve a more holistic view, it’s important to have a well-defined outcome framework that consists of both objective and subjective measurements.
For example, a patient may have a good five-year survival rate but not considering subjective outcomes, we fail to realise that their quality of life is very poor.
On the other hand, a patient may have a very good quality of life but by ignoring objective outcomes, we are unaware of a greater 5-year mortality rate.
But, before you start talking to your stakeholders, you should look on the internet if an outcome framework isn’t already available for your patient population. Don’t reinvent the wheel. Please.
One good source to find an outcome framework is the International Consortium For Health Outcomes Measurement (ICHOM). Other good sources are the National Quality Forum or the National Committee for Quality Assurance (NCQA).
Given that I’m a big fan of ICHOM, I will just focus on this consortium for now. ICHOM is founded by Professor Michael Porter (the VBHC Messiah) in 2012. They have standardized health outcome sets (thus not focused on costs) available for 40 medical conditions on theirwebsite. They have sets for depression & anxiety, diabetes, chronic kidney disease, lung cancer, heart failure and more.
What is an ICHOM standard set? An ICHOM Set is a standardized list of outcomes you should collect based on the patient’s priorities along with instruments and time points for measurement. So concretely speaking a set defines what health outcomes you need to collect when.
Here is an example of the timeline of the standard set for anxiety and depression:
In the standard set, each questionnaire (in this case Baseline Patient-Reported Form, Ongoing Patient-Reported Form and Annual Patient-Reported Form) is explained in-depth:
When they use a validated questionnaire with a validated calculation, scoring instructions are also explained:
How do they develop a standard set? They bring together a multidisciplinary group of patient representatives, leading physicians and registry leaders to prioritize the core set of outcomes. Each set is internationally agreed upon.
Having implemented over 20 ICHOM standard sets myself, I can only say that the quality of their sets is outstanding.
But you know what makes ICHOM even sexier? They took data quality and consistency into account. For each standard set, they have a data dictionary available (excel file). In this dictionary, you can find things like Variable ID, inclusion criteria, timing, reporting source, etc… It’s amazing:
The fact that each organisation that uses ICHOM uses the same variable IDs, ensure that comparison of outcomes is possible. It’s really easy to benchmark data between two organisations that use the same standard set. And it’s so valuable.
So, if you start defining your data framework, please see if an (ICHOM) framework is already available. Don't do work that has already been done for you. If there is no framework available, poor you. Then go out there and talk to all your stakeholders. Find out what they really care about. And if you are lucky and there is a framework available: use this as a basis for your health outcome framework. Combine this framework with other things that aren’t included in the framework (like costs) and validate with your stakeholders whether the outcomes make sense.
While clinical data is great for understanding clinical results (e.g HbA1c, PROMs, PREMs), claim data is crucial as well. So please, don’t forget to collect this data as well. It’s a gold mine and it’s fantastic for understanding visits, procedures, tests…
Step 2: Build a model
Once you have clarity on the outcomes you want to track, you can start building a model to simulate the potential impact you can have on those outcomes.
There are a lot of external databases to build this model. The final goal of this model is to have clarity on the expected return of investment of your digital health solution. For this, it is strongly recommended to develop a test and control group. How is your solution impacting care to someone who is and is not receiving the intervention (your solution)?
Let’s take a look at an example. Imagine you are building a virtual care solution for Asthma patients. Then you should look for data that, for example, answer the following questions:
What’s the total average yearly cost for one asthma patient?
What’s the mortality rate for Asthma patients?
How many % of asthma patients go to the emergency room due to an asthma attack?
Once you found this data, you can start modelling.
How to exactly model this data is way beyond my expertise. If you have any concrete questions about this you should directly contact Tamra. But I’m happy to explain high level what you need to do:
Let’s take the Asthma example again. Imagine 10% of asthma patients have at least one ER admission due to an asthma attack and you know that an average ER admission cost is $1,389. What impact will your solution have on costs if you manage to reduce the ER admission by 25%?
A pulmonology patient's office visit costs on average $135 and an average asthma patient have at least 2 visits per year. What impact will you have on costs if a teleconsultation on your platform only costs $55?
These are all simple examples, you can obviously play with your model and test several cases. What’s my impact if I reduce ER admission by 20%? What’s the impact when I reduce it by 25%? Or 30%?
What’s crucial to mention when building this model is to explain how. How will your solution reduce ER admissions? How will it improve quality of life? How will it increase life expectancy? The answers to those questions are all hypothetical, yes, but it needs to make sense.
Step 3: Insert the data you collected in your model
So now you have your data framework and you started collecting data. Now it’s time to compare your predicted data with your real data. In what ways does it differ? Is it better or worse? Is there an explanation for this? Again, stating the way is crucial.
And whether the data is better or worse, you will need to insert your real data into your defined model and see what impact your solution can have in real life.
Let’s take the asthma example again. In your hypothetical model, you stated that you will reduce ER admissions by 10%, but your real-world data shows a reduction by 15%? Why did you think this happened? Is your statistical power strong enough to state this? And how will this impact your model?
Final thoughts
After all these conversations I've had, I can only conclude one thing: surround yourself with people with tons of experience when it comes to this topic. Seek help, engage with people in digital health communities (like HealthTechNerds) and learn from the mistakes they have made in the past.
Because that's what health care is all about. And that's the beauty of the digital health space: everyone helps everyone. Yes, the competition is big, but the challenges we face and the total addressable markets are bigger. Andy Mychokovsky summarized this perfectly in this tweet:

So don’t be afraid to ask for help, please. Everyone (or almost everyone) in the space is here to help. Let’s focus on collaboration and not competition :-)
—
Rik Renard.
Feel free to connect with me on Twitter or LinkedIn. If you have a comment or feedback you can also send a note to rik@awellhealth.com
Thank you Tamra Lair for taking the time explaining me the basics. And thank you Chris Turitzin and Josh Herung from the HealthTechNerds community for giving feedback.
If you are in the process of proving the value of your digital solution, please contact Tamra. Her expertise in this area is unsurpassed.