How healthcare can use e-commerce tactics to improve patient outcomes
E-commerce players like Amazon, Alibaba or JD.com are masters in optimizing customer journeys. Every touchpoint is tracked, analyzed and improved. All the time.
It made me wonder why we don’t do the same in healthcare. So I asked dozens of e-commerce customers journey experts about their roles and asked what healthcare can learn from these experiences.
What is a customer journey (expert)?
A customer journey is the online pathway people take from the moment they first become aware of a company to the moment they receive an order. This journey may take minutes or months depending on the product or service.
They use website analytics and feedback surveys to map those journeys visually and to identify obstacles and opportunities for enhancing the customer experience.
In a customer journey you have five stages:
Awareness: the customer becomes familiar with the brand through channels, including advertising and word-of-mouth
Consideration: realising that they have a need that must be met, the customer actively considers whether or not to buy the product or service and where to buy it
Purchase: the customer makes the purchase
Retention: the customer uses the product, sometimes seeking guidance from the provider or a user community
Advocacy: the customer spreads the word about the product — whether their opinion is positive or negative
It is logical that companies like Amazon, Alibaba or JD.com continuously optimize their journeys. Competition is huge and if a customer isn’t happy with the service they will never come back.
The difference between e-commerce and healthcare
The shift to healthcare consumerism is already happening. Patients are shifting to D2C companies like Ro, Hims&Hers, Cerebral, etc. where they get a better experience than traditional healthcare. Expectations are higher than ever before. And that’s a good thing!
But patients are not always customers. When you want to buy a television you can choose between Amazon, Best Buy, Walmart… Patients are vulnerable and often have no choices. When you have a heart attack you don’t have time to go shopping or drive 3 hours to the best hospital. You need care. Now. Or imagine you've been suffering from low back pain for months. Before you can have a consultation with a pain specialist, you first need a referral from your GP.
This makes it even more important that we improve the patient experience at every touchpoint during the patient journey. Imagine the impact we can have on care processes if we use the same techniques as an e-commerce player.
I know. It’s impossible to track a patient journey end-to-end. A patient may be treated for her Crohn's disease in a hospital, while for her flu symptoms she booked a teleconsultation via Babylon. And for her depression symptoms, she is using Lyra Health. Fragmentation is real, and will always be real in healthcare.
But what we can already start with is to optimize patient journeys within the same organization. Most digital health players are probably already doing this, but most traditional healthcare providers are not. So here is my 2 cents on what it could look like.
Awareness & Consideration
Healthcare should not spend millions of dollars on marketing. They should invest in scientific evidence to build awareness instead.
Providers must demonstrate for which medical conditions they are the best. It can be cancer treatment, kidney dialysis or palliative care. It does not matter. It’s clear that a provider cannot excel at everything. Patients do not benefit from mediocre care, patients deserve the best care. Again and again.
We need to work toward integrated practise units (IPUs) that are organized around medical conditions over the full cycle of care. Several studies already showcased that IPUs (or focus factories) improve outcomes reduce costs.
An (extreme) example of such a focus factory (or specialised centre) is Shouldice. The only thing they do is non-mesh hernia repair and everything (but really everything) is designed around this.
If the patient has the choice of where to receive care (which is not always the case, see the heart attack example), the patient must be able to objectively choose which healthcare provider is best for their medical condition.
That’s why we need more transparency in our system. Transparency about outcomes. Transparency about costs. This data should be made publicly available and should be benchmarked among all healthcare providers. Outcome and cost variation is a huge, concerning, problem:
We need to collect the same global outcome measures that really matter to patients for the most relevant conditions. On the one hand, this will ensure patients can make informed decisions, but on the other hand, benchmarking and transparency will also lead to improved care processes, quality of service and cost-effectiveness.
For example, after cardiac surgeons in New York State began publishing outcomes data for coronary artery bypass grafting (CABG) in 1989, the state’s CABG mortality rates fell by more than 40%; furthermore, the hospitals with better outcomes saw growth in their market shares.
There is better evidence that transparency influences choice. In Barnsley (England), the local NHS payor gave quality awards to 14 general practices (about 40% of the area’s general practices) because they met certain professional standards. Since 2008, when the awards were introduced, about 4,500 patients (out of a total population of 75,000) have changed their registration to the practices with quality awards.
The atlas of variation from the NHS is a good example of how it can be done. We now need it globally.
Suppose you are going to buy a television, what do you do? You probably start by asking your friends for advice, then you look for reviews on the Internet, and when you have finally decided on a model, you look for a website that can offer you the biggest discount. Why should this be different in healthcare? Healthcare should not be local if the outcomes are much better somewhere else.
Purchase
The 1st thing you need to do to increase patient experience is doing a patient journey mapping exercise. If you go through your own patient journey (can be an onboarding process, having a consultation with a gastroenterologist, etc.), you will immediately see things that can be improved.
These can be small things like magazines from 2007 in the waiting room, or the lack of toys for children. But they can also be clinical inefficiencies in which the care provider questions the patient on paper and then types this info over into the EMR.
For mapping a patient journey you can use different techniques (that’s for another article), but the end result should look something like this:
The most important question you should ask during the patient journey is: what’s the emotional state at each stage and how can we improve this?
Once your patient journey is clear, you first need to define your objectives. For example:
I want to reduce the length of stay at the day clinic by 30 minutes for my patients
I want to increase my departmental capacity by 30%
I want to increase patient experience by 2 points
Once your objectives are clear, you can define what Key Performance Indicators (KPIs) you need at each stage of the patient journey. These KPIs could be things like tacking the waiting times, PREMs, PROMs... My suggestion here is to keep it simple. Only track a maximum of 10 KPIs and make sure those KPIs help your organization track how well you’re are doing to meet your objectives.
Ultimately, you should have a dashboard where you can track these KPIs in real-time:
This dashboard will ensure that you and your team will continuously try to improve your processes. In the best-case scenario, you can also (real-time) benchmark this data against other departments or campuses.
Retention
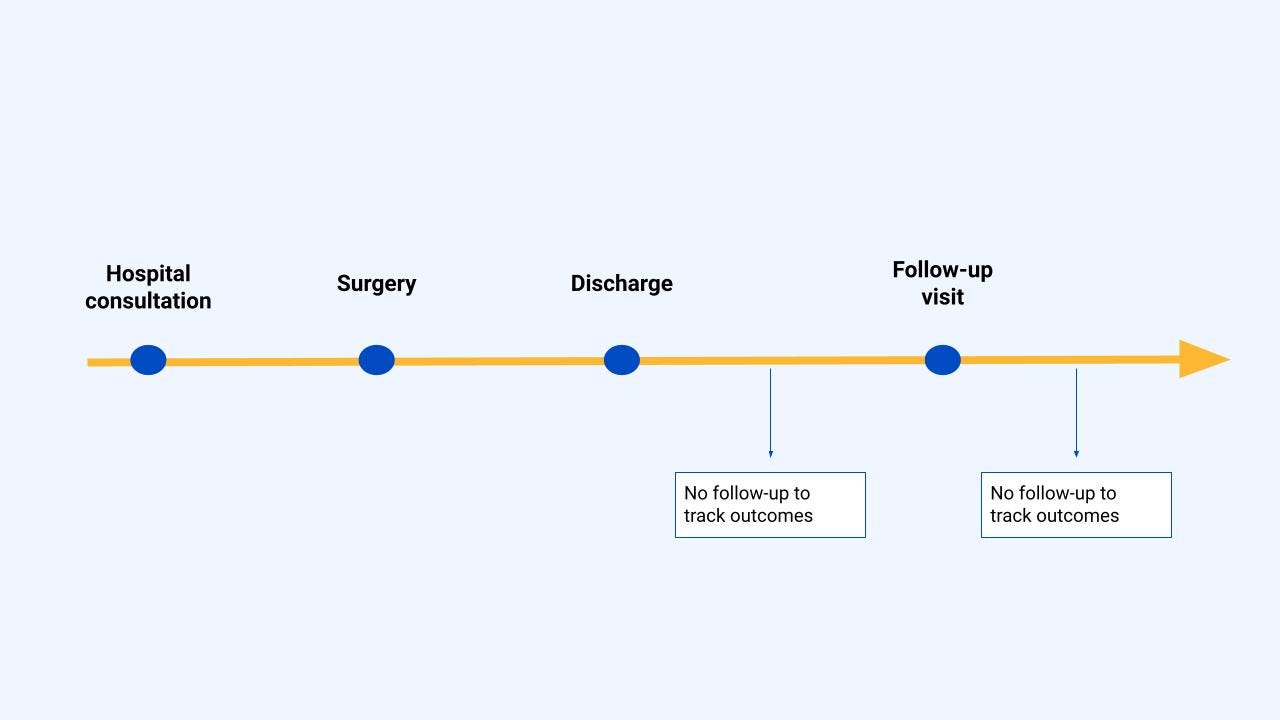
Once the patient received his treatment (e.g surgery, chemotherapy, consultation…), the patient journey often looks like this:
This results in healthcare providers not knowing how the patient is doing between the time of discharge and the next follow-up consultation, leading to sub-optimal outcomes (ER admission, pain, anxiety, etc.).
Therefore, we must adequately follow up and counsel patients with remote patient monitoring (RPM) after the consultation or treatment. When a patient for example reports high fever after chemotherapy, caregivers can take quick actions (e.g share tips on how to reduce fever symptoms) to avoid further implications (like an ER admission). Several studies showed that collecting RPM results in an increased overall survival rate, improved quality of life or decreased emergency room visits and hospitalization.
Another way to support patients throughout their care journey could be setting up a support group, informing them about existing internet forums, sharing information brochures about their disease, developing a self-help program, etc.
Advocacy
Patients are going to talk about their experiences. That’s unavoidable. And patient advocacy will only happen if outcomes are better, costs are less and experiences are better. Finding a balance between these three is one of the most difficult challenges of the moment.
But what’s important to note is that next to better outcomes and reduced costs, patient experience is the third thing to focus on. The third! And this is what a lot of healthcare providers (and digital health) forget. They focus first on experience, and outcomes and cost is a side benefit. You may have hired the best UI/UX designers, but if your outcomes are worse than the competition or the costs is 10x higher than somewhere else you will definitely get bad reviews.
Final thoughts
We will forever have inefficiencies in our healthcare system. But more importantly, care flow improvements are always possible as well. That’s why we need to continuously improve our care flows. We should aim for better collaboration. We should break down silos. We should measure outcomes and costs. And we should have shared responsibilities around the whole patient journey.
So if you believe healthcare can be doing more, you’re not alone. So please, seize every opportunity to improve the patient journey. Small changes over time can really add up. And they can lead to big progress:
And if you're going to improve the patient journey: think of e-commerce for a moment :-)
Cheers,
Rik
—
This is a personal blog. Any views or opinions expressed are my own and do not necessarily represent those of my employer (Awell Health).
Feel free to connect with me on LinkedIn or Twitter. If you have a comment or feedback you can also send a note to rik.renard@hotmail.com