Patient-reported outcome measures (PROMs): the gold standard for outcome improvement
As a healthcare professional, you have probably found yourself wondering how a certain patient of yours is doing, asking yourself questions like:
Did they get better?
Are they responding to the treatment?
Are they experiencing any complications?
Optimal healthcare requires not only that we treat the disease but also that we treat the individual and improve the outcomes that matter to them. It does patients a disservice to focus solely on increasing their life expectancy, while simultaneously decreasing their quality of life.
So how can healthcare professionals, health institutions and governments determine what improved patient outcomes really mean? And more importantly: how can we achieve better patient outcomes?
The best way forward is to get the patients involved in their patient journey through patient-reported outcome measures (PROMs).
What are patient-reported outcome measures (PROMs)?
A patient-reported outcome (PRO) is any report of the status of a patient’s health condition or status relating to symptoms, functionality, mental, social and physical health all from the patient’s perspective without an external interpretation by a healthcare professional.
Patient-reported outcome measures or PROMs (mostly questionnaires and surveys) are the tools used to capture information about PROs. PROMs are self-completed subjective evaluations that can measure health both at a single point in time and over a long period of time.
In 2010, Professor Michael Porter made clear why PROMs are essential:
“Value should always be defined around the customer, and in a well-functioning health care system, the creation of value for patients should determine the rewards for all other actors in the system. Since value depends on results, not inputs, value in health care is measured by the outcomes achieved, not the volume of services delivered, and shifting focus from volume to value is a central challenge.”
As the KCE reported, a distinction can be made between generic and condition-specific PROMs:
Generic PROMs
Generic PROMs are not specific to any particular disease or condition. They often focus on health-related quality of life (HRQoL) or Quality of Life (QoL) in general. Generic PROMs measure things like physical and social functioning, pain, depression or anxiety. They are often used to evaluate the impact of treatment over a longer period of time.
The most commonly used generic PROMs are:
EQ-5D-5L
PROMIS (Patient-Reported Outcomes Measurement Information System)
SF-36 (36-Item Short-Form Health Survey)
Condition-specific PROMs
Condition-specific PROMs measure patient-reported outcomes that are specific to:
Particular disease (e.g. chronic kidney disease, inflammatory bowel disease, Parkinson's disease)
Set of conditions (e.g. cancer)
Domain (e.g pain, anxiety)
Intervention (e.g. hip replacement, appendicectomy, gastric bypass)
Part of the body (e.g. eyes)
These instruments ask questions about the severity of a particular illness or a specific aspect of health (e.g. symptoms after chemotherapy, functional limitations after hip surgery), from the patient perspective. The instruments could also contain more generic elements (e.g quality of life, mobility, daily activities, etc.).
Examples of condition-specific PROMs are:
GAD-7 (General Anxiety Disorder-7)
EORTC QLQ-C30 (European Organisation for Research and Treatment of Cancer Quality of Life Questionnaire)
HOOS-PS (Hip disability and Osteoarthritis Outcome Score)
PHQ-9 (Patient Health Questionnaire-9)
TSK (Tampa Scale of Kinesiophobia)
ACT (Asthma Control Test)
Generic and condition-specific PROMs need to be combined
Both generic and condition-specific PROMs have advantages and disadvantages:
That’s why you always need to combine both generic and condition-specific PROMs for your patient population.
PROMs on Micro-, Meso- and Macro level
The benefits of PROMs
Personalised patient care
PROMs allow healthcare professionals to provide more patient-centred care by gathering information on patients'’ symptoms, health-related quality of life, functionality, recovery and their experience of the disease...
Healthcare professionals spend years acquiring knowledge of diseases. They learn how to treat these diseases, what the most common symptoms are and what the survival rate is for each disease. Yet, despite all the knowledge, they have acquired in medical school and in practice, patients live with the disease on a daily basis. Patients are well-equipped to make decisions related to their care.
With PROMs, healthcare professionals are informed about the patient's experience with their disease. It creates an environment where patients can be treated based on their personal experiences, it facilitates shared decision-making and will eventually improve patient outcomes.
Improved communication between patient and physician
Research carried out after surgical procedures in patients who had prostate cancer during their follow-up through PROMs showed a sixfold improvement in the communication between patients and the healthcare team resulting in prompt and effective intervention.
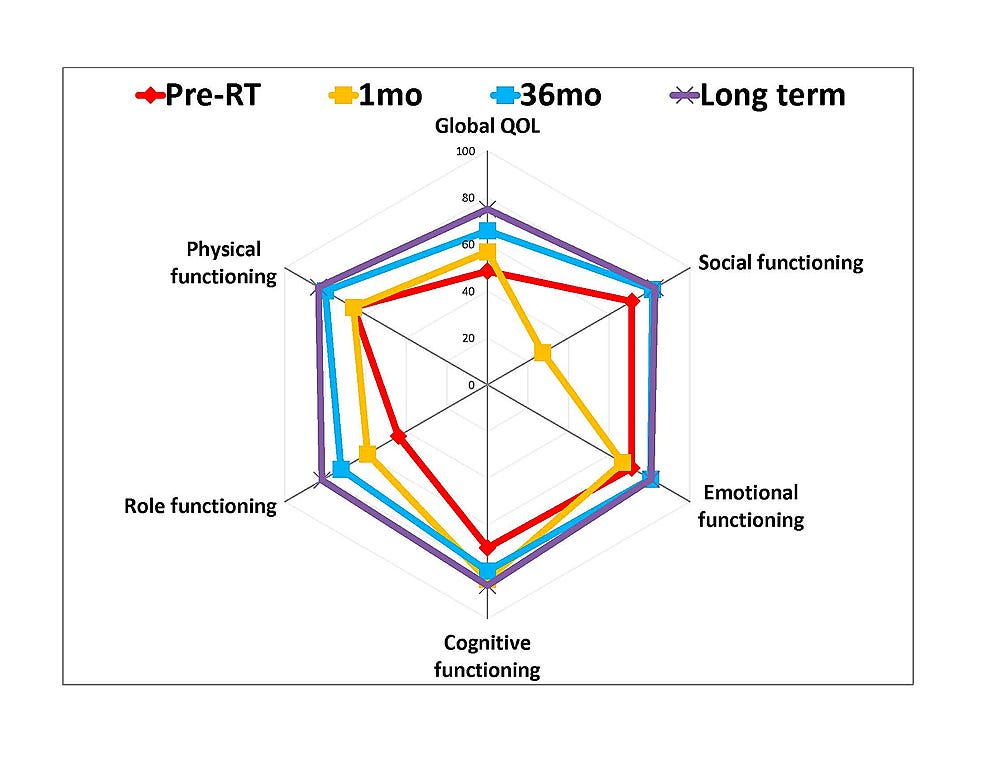
How? A prostate cancer patient walking into a consultation completed the EORTC questionnaire. The physician can consult the results in the following chart:
This chart gives the physician insight into the patient’s disease and their personal experience of the disease improving the communication and understanding between patient and physician. The patient, therefore, plays an active part in decision-making related to their care.
Improved informed decision-making
One of the difficulties healthcare professionals face is patients' inability to give complete and correct information about their health history. PROMs allow patients to provide in-depth information, longitudinal data and a holistic view of their disease which in turn helps healthcare professionals reduce medical errors and death.
This is also provided in an evaluation of PROMs for cancer patients. In this study, 75% of nurses reported improvement in patient care and 65% of oncologists said PROMs help them make better treatment decisions for their patients.
Reduced hospital readmissions and emergency visits
PROMs allow an adequate follow-up of patients with chronic diseases, preventing unnecessary hospitalizations, emergency visits and readmissions. It also reduces the exposure of these patients to nosocomial infections that tend to be fatal.
Through PROMs, hospitals can increase capacity and reduce costs. The KLAS (a healthcare research institution) research report found that digital health monitoring programs reduced the number of emergency department visits by 25% with a 38% reduction in hospital admissions, corresponding to a 17% decrease in costs.
Improved patient outcomes
Besides the four benefits mentioned above, several other studies proved that PROMs can improve other patient outcomes as well:
A study from Basch found that PROMs increased the survival rate for cancer patients by 10%
Long-term PROM follow-up can induce anxiety and fear of recurrence
Howell reported that PROMs enable earlier detection of symptoms
There is evidence that clinicians often underestimate late side effects. The use of PROMs as a dialogue tool, alongside blood samples and imaging, may provide clinicians with more valid and comprehensive knowledge of the patient’s problems
A study has shown that pro-active use of PROMs during treatment improves the QoL of cancer patients
I’m convinced there are several additional studies out there that prove that PROMs drive better patient outcomes.
Conclusion
It’s clear from the examples above that collecting patient-reported outcomes is feasible, improves clinical outcomes and is valuable to patients and clinicians. And although there are a number of challenges while implementing PROMs, there are far more advantages than disadvantages. Every healthcare organization (in-person, hybrid, and virtual) should start collecting PROMs and act upon them. Because providing better care for patients is what we all aim for, and this is exactly what PROMs will facilitate.
—
Rik Renard.
Feel free to connect with me on Twitter or LinkedIn. If you have a comment or feedback you can also send a note to rik@awellhealth.com