Why BPMN doesn’t work for healthcare
This article is a co-written by Thomas Vande Casteele (CEO, Awell). Everyone in healthcare is designing care processes with the objective of driving better outcomes, lower costs or higher efficiency (ideally all three). Care team and product leaders map these care processes in tools like Lucidchart, Excel, Powerpoint or Miro and eventually end up with something like this:

Many care organizations use Business Process Modeling Notation (BPMN) to build these processes, and that's a mistake. Let us explain why.
🤔 Who the f are you
Before telling you why BPMN sucks for healthcare processes, let’s start with a quick summary of our experience with care processes:
We have mapped care processes since 2017
We have implemented 100+ care processes in 20+ care organizations for 50+ different medical conditions (i.e., hip replacement, lung cancer, IBD…)
We have scientific evidence¹* that one of our care pathways improves outcomes (56% higher survival, 27% lower ER admissions) and lower costs (39% capacity increase)
*Although 98% of the credits go to the clinical team <3
🥜 BPMN in a nutshell
If you are already familiar with BPMN, feel free to skip this section and go straight to “Why BPMN doesn’t work for healthcare”.
What is BPMN?
BPMN is a graphical representation of business processes. BPMN's popularity results from its intuitive, visual method of explaining processes, which can be easily understood by all business stakeholders.
Elements of a business process diagram
BPMN has four core elements:
Process flow objects, which include:
Task activities: work that needs to be accomplished (e.g. enter sales order)
Gateways: decision points that can adjust the path of a flow based on certain conditions (e.g. payment ok?)
Events: A trigger to start a process, happens during a process or end a process. It’s something that happened during the process and required a reaction (e.g sales order has been entered)
Pools and swimlanes: visual mechanism of organizing and categorising activities, based on cross-functional flowcharting
Data objects: Allow you to show data flowing through a process (e.g. sales order)
Artifacts: Additional information that is important to the process but does not impact the flow
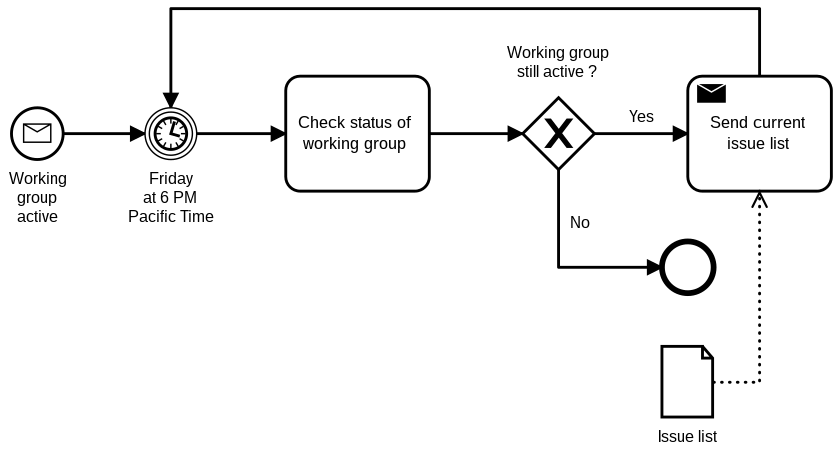
The diagram of the distilled water delivering process below helps explain the above elements:
There is a lot more to BPMN than what I have explained above, so if you’d like to learn more about BPMN you can read “BPMN Method & Style” or “Fundamentals of Business Process Management” or you can watch some Youtube videos about BPMN (it will fuck your algorithm, so I suggest you watch some cute Corgi videos in between).
🚫 Why BPMN doesn’t work for healthcare
BPMN doesn’t work in healthcare because they weren’t built for healthcare. They were built for process automation and managing logistics (i.e., Amazon distribution), not for managing a patient with high blood pressure, diabetes and lung cancer. Healthcare is too complex to effectively leverage BPMN for a few reasons¹:
Many roles participate in one process: nurses, coaches, doctors, dieticians, psychologists, etc.
Several specialists work together on a shared task. e.g. during surgery, you have a head surgeon, different assistants, nurses and other personnel to treat the patient.
A task can be alternatively performed by different roles. e.g. a doctor may perform a task which is usually done by a nurse, i.e., taking blood of a patient.
A task can optionally involve additional roles. e.g. a doctor who may request a specialist on demand for consultation hours.
Every patient journey is unique. You can force standardization in healthcare to a certain level, but several patient-specific factors like medication use, comorbidities or specific patient requests (e.g. a Do Not Resuscitate code) can result in different decisions that deviate from the process.
The problem is that there are some semantics that we need in healthcare that BPMN doesn’t provide, and it makes using it really hard. Simple things like being able to interact with the decision computation while it’s running and to choose a different path (e.g. because patient has comorbidities that are not mentioned in the flowchart) even though the computation tells you should be going this way can’t be done in this BPMN standard.
Let’s say Jane has been hired to help a care team consisting of doctors, care coordinators and therapists map out their care processes. The goal is to be able to tie clinical outcomes back to the care process that was followed and then use insights from that analysis to further improve the processes. Jane starts by interviewing the stakeholders to get to know their current workflow(s). Then Jane begins to map out the care processes in static/non-dedicated tools like word processors (Word, Google Docs), flowchart software (Lucidchart, Draw.io), digital whiteboards (Miro) or presentation software (Google Slides).
In no time, Jane encounters several expectations and conditions at every step of the process. For a patient with severe depression symptoms, you need to plan an appointment with a psychiatrist within 3 days. For an obese patient with severe depression, you need to also involve a dietician. If the patient has moderate depression and is younger than 18 years you first need to get consent from the parents to start treatment, after which they need to be referred to a child therapist.
Jane finds herself trying to draw flowcharts with loads of branches. A quick calculation makes her realize that a disease with four different phenotypes and four different treatments for each of these phenotypes would create a flowchart with 16 branches in the second step of the flowchart.
This example illustrates the unique nature of healthcare processes. Most business processes are predictable and straightforward, but care processes are not and that’s why they cannot be defined as strictly as business processes. This means that flowcharts, and by extension BPMN, is not the right medium to capture healthcare processes.
Think about patients who have been undergoing therapy and become unresponsive to it. This means a change in the predefined process of that therapy. Patients with comorbidities need their treatment adjusted. Or patients that miss their appointment need extra convincing from the care coordinator about the importance of the consultation. Or elderly patients that need help with transportation. In all these cases, the care team draws from the vast knowledge of how previous patients reacted under similar circumstances. Very often, events happen to a patient or a care team that influence the predefined workflow. Failing to represent the variety of paths means we’re failing to support our care team to take the best next step at all times in a patient’s journey.
Yes, a flowchart looks nice on a pinboard and indeed care teams see them literally everywhere as it is an attempt to tame the variation in real life and bring it back to simple processes that can be controlled. But this effort is futile. Flowcharts and BPMN cannot reflect the whole care process and its variations in practice. In most cases, the multidisciplinarity of a care team, different patient characteristics or sudden changes in circumstances are not taken into account. Thus, what's needed is a modelling language that can capture and incorporate this complexity and the knowledge within the healthcare workflows in a better way.
😇 Is BPMN really useless in healthcare?
We must admit, the above lacked some nuance. You can do some basic things with BPMN in healthcare (e.g. send a reminder for an appointment to decrease no-show rate), but the vast majority of processes in our industry are just not basic.
So yes, you could use BPMN for mapping basic processes but if your processes become a bit more complex you’ll need another modelling language. Our systems already have quite some (understatement) difficulties communicating with each other (our assumption is that the 101 different data standards we have might have something to do with this), so let’s try to not have our processes mapped in different languages, please.
🩹 What’s the fix?
There are some incredibly smart people working on a new language for care processes and yes (!) that will be the subject of the next blog post. What I can already tell you is that the solution is not using multiple colours for one task lol.
This is not the solution lol
See ya nerds*!
Rik Renard & Thomas Vande Casteele
PS: We will be in Boston, New York & Las Vegas (HLTH conference) in the coming weeks, ping me (rik@awellhealth.com) if you want to grab a coffee
PSS: I try to be funny on Twitter, feel free to follow me
PSS: Thank you Joe Mercado and John Klaus for proofreading
*Sorry for calling you a nerd, but my assumption is that whoever reads this is an actual nerd no?
¹ Demedts, I., Himpe, U., Bossuyt, J., Anthoons, G., Bode, H., Bouckaert, B., Carron, K., Dobbelaere, S., Mariën, H., Van Haecke, P., & Verbeke, W. (2021, December). Clinical implementation of value based healthcare: Impact on outcomes for lung cancer patients. Lung Cancer, 162, 90–95. https://doi.org/10.1016/j.lungcan.2021.10.010
²Müller, R., & Rogge-Solti, A. (n.d.). BPMN for Healthcare processes.
.